LONG CASE- FINAL PRACTICAL GENERAL MEDICINE
I have been given this case to solve in an attempt to understand the topic of patient clinical data analysis to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
Name : R. AKHIL CHANDRA
Batch: 2017
Hall ticket number: 1701006149
Chief complaints:
A 22 yr old female, who is a farmer by occupation, studied upto 10th standard, came to the OPD with the chief complaints of-
*Generalized swelling of the body since 5 days
*No urine output since 5 days
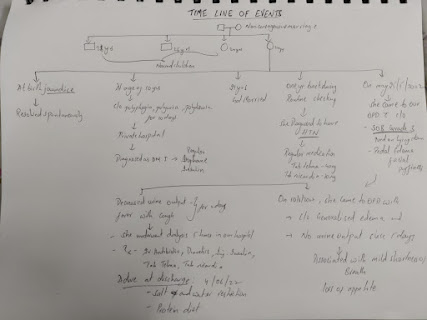
History of presenting illness:
-She was apparently asymptomatic 5 days back then she noticed swelling of the body , initially involving the face and periorbital region ,later legs from ankle to thighs and also upperlimb and abdomen.
-Swelling was insidious in onset, gradually progressive and associated with pain .no aggravating and relieving factors.
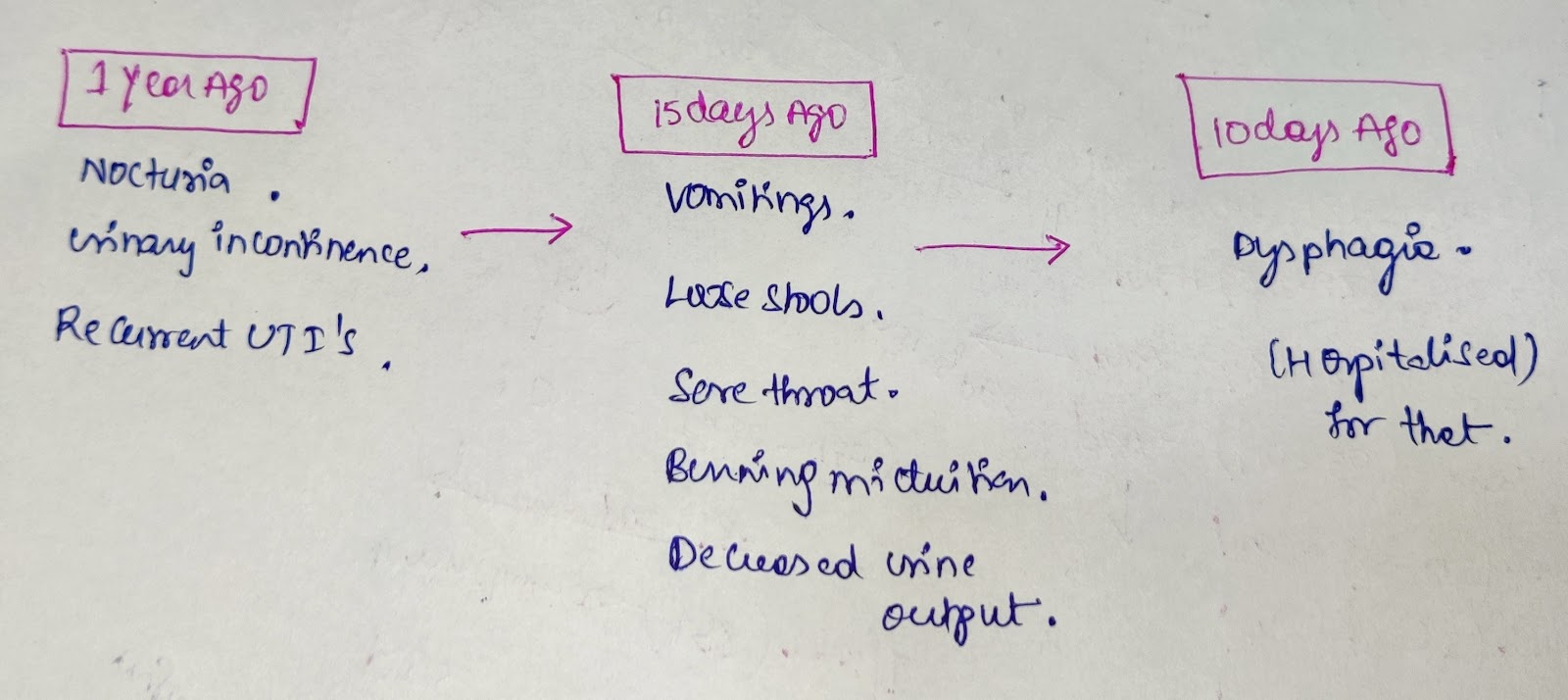
-No urine output since 5 days , initially there is decreased urine output for 2 days followed by no URINE OUTPUT.
H/o loss of appetite since 10 days
H/o blurring of vision, for which she has been provided spectacles.(15 day ago)
No h/o burning micturition and dysuria
No h/o fever ,rash and abdominal pain
No h/o nausea , vomiting, headache.
No h/o chronic cough, hemoptysis and weight loss.
No h/o bone pain
No h/o pins and needles sensation in foot
Past history:
She is k/c/o Diabetes since 12 YEARS on regular medication (isophane insulin)
K/c/o Hypertension since 1 year on medication (tab .Telma 40 mg and tab .nicardia 20 mg)
No h/o TB, asthma, CAD, EPILEPSY, thyroid disorder.
FAMILY HISTORY:
NO h/o Hypertension, diabetes in the family members.
PERSONAL HISTORY:
Diet: mixed diet
Appetite: decreased
Bowel and bladder: bowel is regular but bladder -no urine output since 5 days
Sleep - adequate
GENERAL EXAMINATION:
after taking consent from patient, she is examined in a well lit room and after adequate exposure.
She is conscious, coherent, cooperative
She is moderately built and poorly nourished.
She is oriented to time, place and person
On examination she has pallor.
No icterus, clubbing, cyanosis, lymphadenopathy
There is oedema (pitting TYPE)
VITALS:
•TEMPERATURE: febrile @time of examination
•PULSE:100 BPM
•RR:20 CPM
•BP :140/90 mm of hg , measured in supine position and in left upper arm.
•Spo2-97%
•Grbs-220 mg/dl
SYSTEMIC EXAMINATION:
*PER ABDOMEN;
#INSPECTION;
Shape of ABDOMEN- round and distended with flank fullness
No visible scars and sinuses
No visible engorged veins
Umbilicus is inverted and central in position.
#PALPATION;
SOFT and non tender
No organomegaly.
*Fluid thrill is present.
#Percussion;
Dull note heard over the abdomen
#AUSCULTATION;
Bowel sounds are heard normally
No bruit heard
*RESPIRATORY SYSTEM;
ON inspection,shape of chest is B/l symmetrical
Movements of chest -equal on both sides
Trachea appears to be in central position
On PALPATION,there is decreased movement of chest over both lower lobes ( infra axillary and infra scapular)
Vocal fremitus -decreased in IAA,ISA on both sides
ON Percussion thers is Stony dull ness over IAA,ISA on both sides.
On AUSCULTATION; absent breath sounds over ISA,IAA .
NVBS heard above the dullness.
Vocal resonance is also decreased over both lower lobes.
*CVS;
S1,S2 heard ,no murmurs,jvp is normal.
*CNS; intact
Higher mental functions are normal
No meaningeal signs
Motor and sensory systems are normal
Gait is normal.
PROVISIONAL DIAGNOSIS
#DIABETIC NEPHROPATHY with bilateral PLEURAL EFFUSION.
INVESTIGATIONS ON 10/6/22
#CBP:
•Hb;6.5gm/dl
•RBC count:2.42millions /cumm
•TC:7100cells/cumm
Neutrophils;70%
lymphocytes;17%
MCV:80.2fl
MCH:26.9pg
MCHC;33.5%
RDW-cv;14.2%
Platelet count:1.20lakhs/cumm
•Smear:normocytic and normochromic
#CUE:
Color -pale yellow
Appearance-clear
Reaction -acidic
•ALBUMIN-3+
•PUS CELLS :4-5
•RBC: absent
•Casts : absent
#BLOOD UREA:110mg/dl
#SREUM CREATININE:6.2mg/dl
#SREUM electrolytes;
Na :136mEq/l
K:3.5mEq/l
Cl:97mEq/l
#SEROLOGY;
*HbsAg; negative
*AntiHCV antibodies;non reactive
*HIV 1/2 rapid test ;non reactive
#USG : FINDINGS
*B/l grade 2 RPD
*Gross ASCITES
*B/L MODERATE to gross PLEURAL EFFUSION.
#CHEST XRAY;
#2DECHO;
Investigations on 11/6/22.
Hemogram:
•Hb-6.2g%
•Blood urea-127 mg/dl
•Serum creatinine -6.7mg/dl
Treatment;on 10/6/22
-Inj.lasix 60mg/iv/BD
-Inj .human actrapid insulin.6U/iv/stat
-Insulin infusion 6ml/hr
-Tab.nicradia 20 mg /po/BD
-Tab .Telma 40 mg/po/OD
-NBM till further orders
-Fluid and salt restriction
-Grbs monitoring hrly .
#Treatment on 11/6/22:
-Inj. lasix 60 mg /iv/BD
-Inj insulin infusion 6ml/hr
-Tab.nicardia 20 mg/po/bd
-Tab. Telma 40 mg/po/oD
-NBM till further orders
-Fluid and salt restriction.
-Grbs monitoring hlry
Investigations on 12/6/22
•Blood UREA:68mg/dl
•SERUM CREATININE: 4.5mg/dl
Treatment on 12/06/22:
-Inj.lasix 60 mg/iv/BD
-Inj human actrapid S/c
-Tab.nicardia 20 mg /PO/BD
-Tab.Telma 40 mg/PO/OD
-Fluid and salt restriction
-Bp/PR/Grbs 4th hourly
-inj.piptaz 4.5mg/iv/stat
-inj.piptaz 2.5gm/iv/TID
Treatment on 13/06/22:
-Inj Piptaz 2.5gm/IV/TID
Inj Lasix 60mg/IV/BD
-Inj Human Actrapid S/C acc to GRBS
-Tab Nicardia 20 mg/BD
-Tab Telma 40mg/OD
-Tab Orofer XT PO/OD
-Tab Nodosis 500mg/BD
-Tab Shelcal 500mg/OD
- BP, pulse rate, temp 4th hourly




.jpeg)



.jpeg)

Comments
Post a Comment